Keep reading and we'll explain what happens to waste from medical procedures once it has been collected.
When a red biohazard bag is tied off in a hospital, most people never think about it again. But that bag begins a highly regulated journey—one that protects public health, the environment, and the people handling it.
What actually happens to medical waste after it’s collected?
TriHaz Solutions will explain.

What Counts as Medical Waste?
Medical waste, also known as clinical waste, includes a wide range of materials generated as a by-product of healthcare activities. These might be:
- Sharps (e.g. needles, scalpels)
- Infectious waste (e.g. contaminated dressings)
- Anatomical waste (e.g. human tissue)
- Pharmaceutical waste (e.g. expired drugs)
- Cytotoxic and cytostatic waste (e.g. chemotherapy agents)
- Chemical waste (e.g. disinfectants)
- Offensive waste (non-infectious but unpleasant)
Each of these categories must be managed differently, and failure to do so can lead to contamination, injury, or legal consequences. But how does that separation happen in practice?
Collection and Transport
Once medical waste is properly segregated, labelled, and sealed, the next critical phase begins: collection and transport. This isn't a simple courier service, it's a chain of custody that must be airtight from start to finish.
Licensed Haulers with a Mission
At facilities like ours, we rely on licensed medical waste haulers such as TriHaz Solutions, whose drivers aren’t just delivery personnel, they’re trained biohazard specialists. Each driver is certified in handling regulated medical waste, including infectious, cytotoxic, and sharps-related materials.
They operate under strict procedural oversight, ensuring that every pick-up aligns with cradle-to-grave waste tracking. What happens to medical waste means each container is logged, traced, and accounted for until its final destruction—ensuring no waste goes unmonitored.

Vehicle Standards
The vehicles themselves are subject to rigorous regulation. These aren’t generic, they’re purpose-built with:
- Leak-proof interiors to contain any spills
- Lockable compartments to prevent unauthorized access
- Clear hazard labeling for instant recognition in case of emergency
- Temperature controls where needed, especially for pharmaceutical or pathological waste
Transport vehicles undergo regular inspections, and any deviation from regulatory standards results in immediate suspension from service. That's the reality of what happens to medical waste.
Real-World Insight Into What Happens to Medical Waste
Collection isn’t done randomly. Our schedules are calibrated to ensure waste never accumulates beyond safe storage limits. In high-output environments like hospitals or research labs, we may have daily collections, while smaller clinics might operate on a twice-weekly rotation.
Our team collaborates closely with the haulers, often coordinating pickups around peak usage times to ensure continuous flow and minimal on-site storage.
The journey of medical waste doesn't end at collection, it continues at specialized treatment facilities, where the focus shifts from containment to neutralization. This is where science meets engineering to ensure harmful materials are rendered harmless before final disposal.
Each type of waste demands a specific approach, depending on its composition, risk level, and volume. Here's how expert facilities like ours determine the best path forward.

Incineration
For pathological waste (human tissue, body parts) and many pharmaceuticals, incineration remains the gold standard. At high temperatures exceeding 1,000°C, organic materials are reduced to ash, and infectious agents are obliterated.
- Why use it? Complete destruction leaves no biological trace.
- Impact: Reduces waste volume by up to 90%, making long-term storage or landfill unnecessary.
- Compliance Note: Emissions are closely monitored under environmental regulations, with modern incinerators using scrubbers and filtration systems to minimize pollutants.
Autoclaving
Infectious waste, often labeled “red bag” waste, is typically treated through autoclaving, a high-pressure steam sterilization method. This is how TriHaz handles most of their medical waste.
- Use Case: Gauze, gowns, gloves, culture dishes, and other non-sharp contaminated materials.
- Process: The waste is exposed to pressurized steam at ~134°C for 30–60 minutes.
- Result: Once sterilized, the waste is considered non-infectious and may legally be landfilled under local waste codes.
Facilities that handle high volumes of general clinical waste use autoclaves daily, often with automated systems to improve efficiency and reduce human contact.

Chemical Disinfection
Some wastes, particularly liquids or microbiological cultures, are unsuitable for incineration or steam sterilization. That’s where chemical disinfection comes in.
- Common agents: Chlorine-based solutions, hydrogen peroxide, enzymatic cleaners.
- Process: Waste is immersed or treated in secure tanks, ensuring complete microbial kill before disposal.
- Caution: Staff must be trained in handling reactive substances, and ventilation is critical.
This method is particularly common in research institutions and diagnostic labs, where contamination risks are high, but autoclaving isn’t always appropriate.
Advanced Alternatives
In recent years, a wave of advanced treatment technologies has emerged, offering lower-emission, high-efficiency alternatives:
- Microwave Disinfection: Pulsed microwave energy heats waste from the inside out, sterilizing it without combustion.
- Ozone-Based Systems: Ozone gas oxidizes pathogens, breaking down biological contaminants at the molecular level.
- Encapsulation: Waste is embedded in solid polymer blocks, immobilizing hazardous components prior to landfill.
These innovations are especially valuable in settings seeking lower carbon footprints or operating in regions with strict air pollution limits.

Final Disposal
Even after medical waste has been treated and neutralized, its journey isn’t over. The final disposal phase is where treated materials are either safely buried, repurposed, or—occasionally—stored under strict environmental control. But unlike ordinary waste, nothing here is done casually. Every gram is documented, and every step is governed by both federal and state law.
From Sterile to Landfill
Autoclaved waste, now rendered non-infectious, is often visually indistinguishable from standard municipal waste—but its disposal is still regulated.
- Destination: Sanitary landfills approved to accept treated medical materials.
- Pre-Disposal Step: Many facilities shred or compact autoclaved waste to reduce volume and eliminate recognizability.
Facilities must retain documentation showing that the waste has been sterilized to required parameters—time, temperature, and pressure—all logged and auditable.
Ash Disposal
When waste is incinerated, it doesn’t disappear—it transforms. The resulting ash may still contain trace elements of heavy metals or pharmaceuticals, and as such, it demands specialized handling.
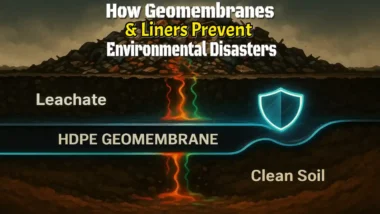
- Destination: Ash monofills—engineered landfills designed specifically for combustion by-products.
- Environmental Controls: Leachate collection systems, impermeable liners, and groundwater monitoring are standard.
Some jurisdictions allow stabilized ash to be used in industrial applications, such as cement or asphalt, but only after rigorous testing confirms it meets safety thresholds.
Treated Sharps
Sharps waste, after being autoclaved or chemically disinfected, undergoes one final safety measure—mechanical shredding. This not only prevents reuse (a serious risk in some parts of the world) but also ensures the waste can be safely compacted for landfill.
- Post-Treatment: Shredded material is visually inspected and sealed in secondary containers.
- Disposal: Sent to municipal landfill, often with a separate designation from general waste.
Documentation and Compliance
Behind every correctly disposed container of medical waste is a stack of documentation proving it was handled safely, legally, and ethically. In the world of regulated waste, paperwork isn’t just bureaucracy—it’s protection.
Whether you're a hospital, lab, or outpatient clinic, maintaining a complete and accurate audit trail from the point of generation to final disposal is non-negotiable.

Core Documents You Must Maintain
Here are the key records facilities are required to generate and retain:
- Manifests & Tracking Forms:
These are the cornerstone of cradle-to-grave tracking. Each time waste changes hands—from generator to hauler to treatment site—a signature and timestamp are logged. This provides a verifiable chain of custody. - Weight and Volume Reports:
These logs track how much waste is produced over time, broken down by category (e.g., sharps, infectious, pharmaceutical). This helps with trend analysis, budgeting, and sustainability efforts—and is often required for annual reporting. - Treatment Verification Logs:
For every load treated via autoclave, incinerator, or chemical process, logs are generated to confirm that correct parameters (temperature, duration, chemical concentration) were met. These are especially critical during audits or inspections.
Why It Matters
- Regulatory Compliance:
Federal agencies like the EPA, OSHA, and DOT, as well as state-level environmental health departments, can inspect facilities without notice. Gaps in your records can result in steep fines—or worse, shutdowns. - Legal Liability:
If improperly treated waste causes harm—whether through accidental exposure or environmental contamination—your documentation will be your first and best defense. - Operational Clarity:
These records also help facility managers spot inefficiencies, overuse, or errors in the waste stream—empowering smarter decisions and safer processes.
Retention Requirements
Retention periods vary by jurisdiction, but a general rule of thumb is:
- Manifests: Retain for a minimum of 3 years
- Treatment Records: Typically 3–5 years, depending on state law
- Training Records (linked to compliance): Often up to 5 years
Facilities are increasingly using digital waste management systems that auto-generate these documents, notify staff of upcoming collection windows, and flag anomalies. It’s an investment that pays off in both safety and peace of mind.